Provider Sentiment Around Prior Authorization
| Jessica Behrendsen

Prior authorization (PA) has long been recognized for its ability to help payers manage prescription coverage while ensuring appropriate, safe treatment for patients.
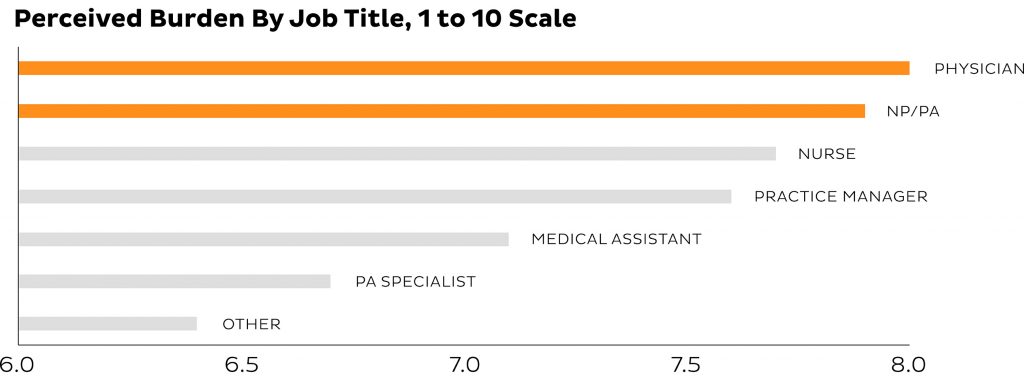
While a necessary component of the healthcare industry, PA is often cited as one of the top burdens for healthcare professionals. In fact, the average burden reported by providers around PA is a combined 7.7 on a 10-point scale.1
“I spend hours on the phone, especially after the New Year. It’s so very time consuming when I could be working on more important things such as stat appointments or vitals.”
― Health care provider
Beyond causing frustration for pharmacists, providers and their staff, the perception of PA negatively impacts relationships between stakeholders in the industry. Providers associate a poor PA experience with payers, and often change their prescribing behavior, potentially impacting patient health outcomes, to avoid the PA process. That being said, providers and payers want to work together to make this process easier for all stakeholders, and find solutions which will benefit the patient.2
Ultimately, the patient – arguably the most important customer for payers, providers, pharmacists and manufacturers – bears the brunt of the PA process through delayed treatment or prescription abandonment.
In this article, we’ll take a deeper look at the factors that cause PA to be perceived negatively by providers, and how industry stakeholders can improve the process with an ePA solution. By doing so we allow physicians and their staff to focus on treating patients and improving medication adherence.
Who is responsible for the PA process?
A common misconception is that prescribers handle PA requests. In fact, seventy-two percent of requests are managed by medical assistants, nurses or PA specialists.3
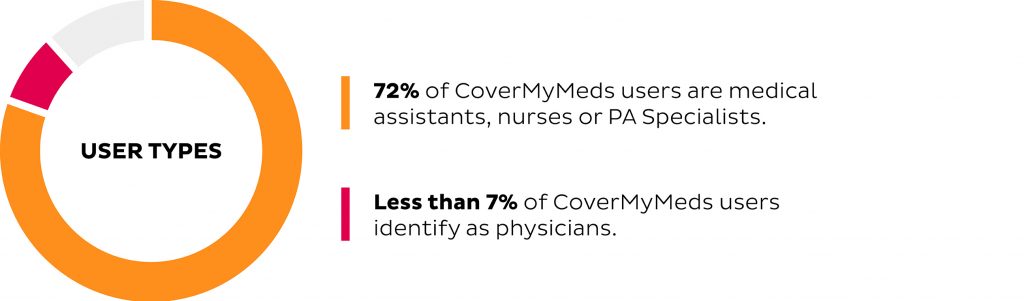
Prior authorization is not an explicit component of the job for clinical staff, and is often passed around to different employees based on who can fit the task into their busy day. In fact, nearly 30 percent of CoverMyMeds users report that their office lacks a formal process for handling their PA workload.4
Physicians feel the greatest pain from PA
While physicians reportedly spend the least amount of time on PA per week, they also reported the highest level of perceived burden. On a scale of one to 10, physicians rank PA as an eight.
On the other end of the clinical spectrum, PA specialists rank the burden of PA as 6.8 out of 10.5 Data indicates that the burden of PA increases with clinical responsibilities, likely because those individuals prefer to spend more time with patients and have less time for administrative tasks.
Qualitative data from physicians supports that beyond impacting their time with patients, providers view the PA process negatively because it’s perceived as questioning their judgement on how best to treat a patient.
“I prescribe a medication based on my clinical judgement. To have non-medical people require me to spend an inordinate amount of time justifying my medical decision takes time away from patients.”
― Health care provider
In addition to reducing the administrative hassle of PA requests, electronic solutions like CoverMyMeds provide healthcare professionals a one-stop-shop for all PA needs. According to providers, one of the top reported benefits is the ability to handle PA requests for all drugs and all payers through CoverMyMeds.
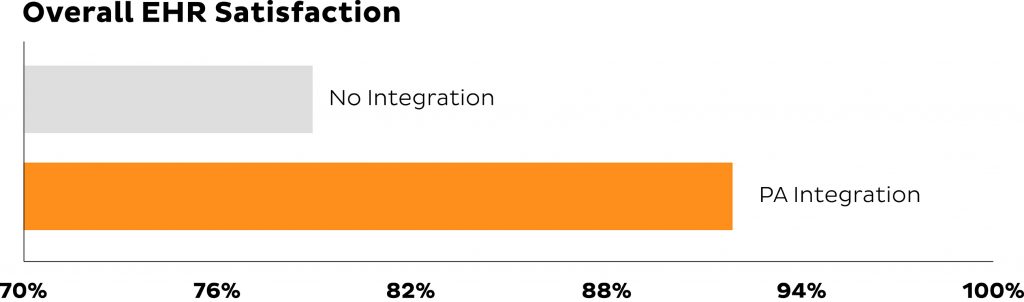
When providers initiate PA requests within their electronic health record (EHR) system at the point of prescribing, the process is further streamlined for all stakeholders. This allows PA to be managed proactively and automates the bulk of the work when preparing to submit the request, which is often completed by a PA specialist or medical assistant. In fact, in a recent survey with representative providers, 92 percent indicated greater levels of overall satisfaction with their EHR when it had the functionality to handle PA requests.6
“I like that [CoverMyMeds] pulls in the request for me and I don’t have to search for it on the internet. Also, I like that I don’t have to write it all down, I can just fill out the request online and send it right from the computer. Saves me time.”
― Health care provider
Electronic Prior Authorization Improves the Prescribing Experience and Patient Treatment
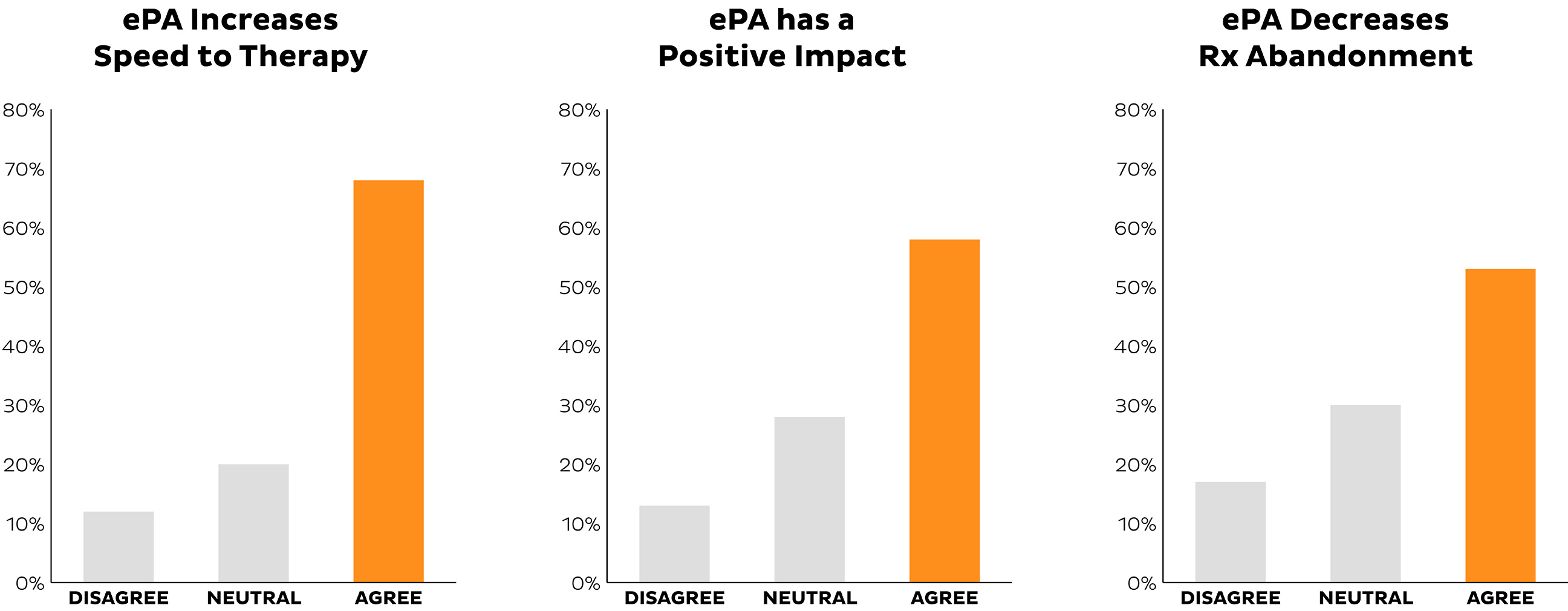
While providers universally agree on the burden of PA, they are equally aligned on the benefits of ePA and count on healthcare stakeholders to provide PA support that allows them to make clinically appropriate decisions on how to treat their patients.
Data indicates that without an ePA solution for providers, 38 percent of patients receive therapy as originally prescribed. With the assistance of a solution like CoverMyMeds, more than 51 percent of patients were successful in receiving therapy as originally prescribed by their physician.7
Providers agree that ePA can increase speed to therapy for a patient, positively impact the workflow of their staff and most importantly, decrease the likelihood of prescription abandonment.
More patients get the medication they need to live healthy lives when industry stakeholders support ePA solutions and partner with CoveryMyMeds. Learn more about CoverMyMeds ePA solutions.
- The ePA National Adoption Scorecard
- Fierce Exclusive — How payers are building better relationships with their network partners
- CoverMyMeds Survey Data
- CoverMyMeds Survey Data
- The ePA National Adoption Scorecard
- CoverMyMeds Survey Data
- The ePA National Adoption Scorecard